Concerned About Healthcare Worker Resilience? Ask These 6 Questions
Ask these six questions to help you support frontliners and healthcare workers, and put them in the best position to help patients.

We’ve created an e-book to help you navigate the three stages of a crisis with the right workforce questions and data analysis. Download it here. You may also find this checklist on Key Questions to Answer During a Crisis handy. Check it out at this link.
Fostering healthcare worker resilience is a major challenge in the midst of a pandemic.
At the most fundamental level, frontline staff need an adequate supply of physical tools to feel safe and supported. They also need to be heard by their employers and supported by the right team. And as healthcare organizations grapple with a surge in demand for services, people need to be protected from crippling workloads.
For example, a 2017 study revealed that: “Nurses who experienced heavy workloads on a daily basis were 3.5 times more likely to report high emotional exhaustion than nurses who experienced heavy workloads less frequently.” By asking the right questions about overtime hours, organizations can ensure the work is more evenly distributed among staff.
This is just one of the ways healthcare organizations can mitigate COVID-19’s psychological toll on frontline staff with better workforce decisions. Here are six questions you can ask of your workforce data that will help you support people on the front lines–and put your healthcare teams in the best position possible to serve patients:
Question #1: Are we prepared to meet a surge in demand?
Having a plan ready to address unexpected surges is essential–even if your organization has already experienced one. Until a vaccine becomes available, the virus will return, prompting more outbreaks. The exposure to prolonged stress may further impact the resiliency of healthcare teams.
To help organizations prepare and prevent teams from becoming overwhelmed, Providence St. Joseph Health (PSJH) has released a COVID-19 Clinical Staff Projection Calculator. This calculator takes your estimated bed counts and staff ratios and produces the size and type of workforce needed to care for an influx of critical care patients. (You can access the calculator here.)
Another resource is the Visier COVID-19 case data found on GitHub. The dataset includes COVID-19 cases, fatalities, and recoveries with global coverage and granularity for many countries.
Question #2: Do we have a mix of experience levels on our shifts?
On any given shift, the presence of more experienced nurses and doctors–who can provide the needed support for junior team members–can go a long way in reducing work-related stress.
To ensure you have the right mix of experience levels on your team, look at your headcount data to understand: Who has been at this particular facility the longest? How long have they been practicing? Once you have identified those experienced team members, you can ensure they are evenly distributed among schedules.
Variety in tenure creates more optimal teams, and so does the right occupation mix. This will be easier to determine if you have combined data from multiple people and operational systems so that headcount, people costs, and overall productivity can be analyzed in one place, by many people, in real time.
Question #3: How supported do frontline workers feel?
Many organizations have implemented regular pulse surveys to better understand and respond to the concerns and needs of frontline workers. They are prompting staff to answer questions such as:
Am I getting the support needed to give optimum care?
Am I getting adequate rest periods?
Do I get counseling services on the tough cases?
If I have at-risk people at home, do I have financial support to live elsewhere?
It is also important, however, to act on what the organization hears back from employees through this process. Some organizations, hearing that healthcare workers are concerned about infecting their families, have offered to pay for hotel stays when the virus is at its peak. Conducting short pulse surveys and then acting on results shows that the organization cares for the well-being of its workers during this extreme crisis.

Visual showing the trend of productive hours recorded to employee engagement results. Fictional data used for illustrative purposes.
Question #4: Is there an adequate supply of back-fill for our people?
With so many healthcare workers facing brutal realities, it might not seem like the experience of back-office recruiting teams should be a priority. However, the more quickly the organization can make and on-board new hires, the less overwhelmed doctors and nurses will be.
Healthcare recruiter burnout is a real possibility in this pandemic. Organizations have been scrambling to recruit for registered nurses, physicians, respiratory therapists, and patient care technicians. At one organization I spoke with, they were trying to interview people within 48 hours of an application being submitted.
This is where your data can help. If you see that your hires-per-recruiter metric is too low, for example, you can ask: “What if I add more recruiters to deliver the required volume?” and model the cost scenarios to come up with sound and creative plans.
Question #5: Is overtime putting our people at risk of attrition?
Healthcare leaders can look at hours worked to identify whether any employees are working too much, which may cause fatigue, burnout, and poor performance. Specific questions covered here can include: Who has worked the most hours recently? Is overtime evenly distributed or concentrated among a few employees?
The following questions related to absenteeism can also help you assess whether people are working too much:
Which employees have high recent absenteeism?
What is the relationship between absenteeism and overtime?
What is the relationship between absenteeism and turnover?
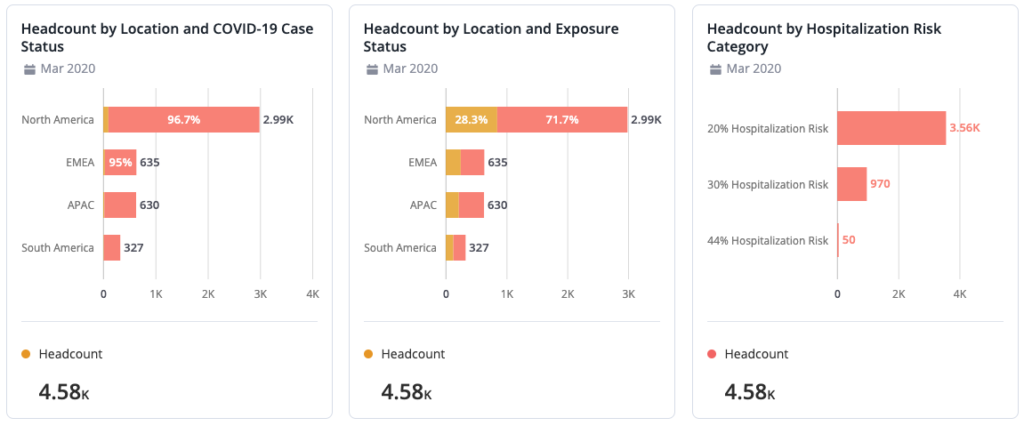
These analyses show headcount statuses according to COVID-19 exposure, location, and risk categories so talent managers can stay on top of absences. Fictional data is used.
Of course, absenteeism can stem from more than just overtime. High levels of absenteeism could also be an indicator of an acute health condition, family, or personal issue for which the organization may be able to provide support.
To better understand this, some organizations are tracking the reasons why people are taking time off, differentiating vacation time from time taken to support a personal matter (such as PTO for childcare due to school closures). Some organizations are tracking reasons for sick time as well, differentiating regular sick time vs. COVID-19 sick time. By gathering this granular information, leaders can see which issues are a priority and need to be addressed.
Question #6: Are we making the best use of the skills we have?
Redeploying people within the organization to areas where their skills are needed most is another way to lighten the load of people on the front lines. For example, if elective surgeries have been delayed, there may be medical healthcare professionals who can be reassigned to new roles within the organization. Instead of furloughing these people, ask how their skills might be in demand.
During our recent healthcare open forum, one healthcare panelist discussed a need to segment the workforce and identify whether workers could be transitioned to frontline and essential activities. Specifically, they needed to identify those who could work in the ICU to operate a ventilator or vacuum floors.
This required the organization to assess skills and whether certifications were up-to-date. To get this information, they supplemented their skills taxonomy with survey data to collect license information, for example. From this, they could provide shortlists of those most able or quickly able to serve. This collection of data is now serving as a framework for collecting data from new hires to ensure they can address future virus surges.
This example shows that, by gaining visibility into employee profiles and talent data, you can make better decisions to shift resources to new areas of the organization. Determining where there can roles be reassigned to areas that are experiencing a greater demand is key.
Helping the helpers with better workforce decisions
This is not only a healthcare crisis–but a mental health crisis too. Reports on the psychological impacts of COVID-19 reveal that healthcare workers are experiencing elevated levels of anxiety, stress, and fear. Poor healthcare worker well-being has also been associated with poor patient safety.
When healthcare leaders deploy their resources in the most optimal way possible, it has an impact on the individual frontline worker’s experience. A silver lining in this very dark cloud is that, by shedding a light on healthcare worker well-being, we can better support healthcare workers–now and long after the pandemic has passed.